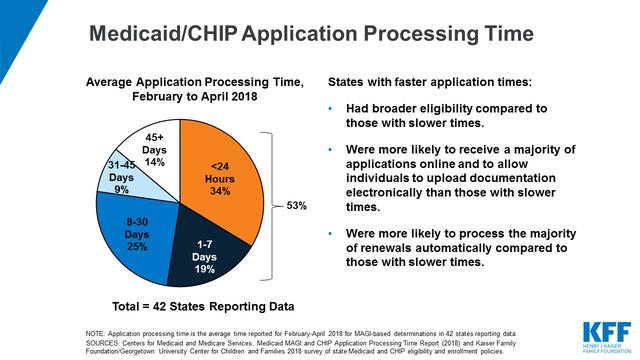
Both Medicaid and the Children's Health Insurance Program (CHIP) provide healthcare coverage for low-income children. In 2018, 36.3 children were enrolled in Medicaid and 9.6 million in CHIP. With nearly 46 million children accessing health care through these programs, it is important to understand how they work.
Both programs are jointly funded by federal and state governments. Both are run by the states. There are still some inherent differences between the two programs you need to understand if you have a child in need of health care. Simply put, it depends on what state you live in.
Medicaid Eligibility for Children
Children raised in families earning 138 percent or less of the federal poverty level (FPL) per year are eligible for Medicaid. The FPL is calculated by the U.S. Department of Health and Human Services every year and is based on the number of people in a family with consideration also given to location. After all, some states are much more expensive to live in than others, like Hawaii.
Before the Affordable Care Act (ACA), i.e., Obamacare, was passed in 2010, children became eligible for Medicaid based on both their age and family income. Generally speaking, the older a child got, the less likely he was to get Medicaid coverage for the same family income. Oddly enough, this meant that only some children within the same family might be covered in any given year. The new legislation made the income eligibility standard the same for children 0 to 19 years of age.
Some states still have different eligibility requirements for different ages groups, but the standard value is now set for at least 138 percent of the FPL for all children. Before the ACA, the eligibility threshold was set at only 100 percent for children between 6 and 19 years old.
Eligibility for CHIP
Medicaid is intended to provide care for the poorest children. The CHIP program was established in 1997 as a way to expand coverage to children who have lower family incomes but who fall outside the Medicaid eligibility window.
The states ultimately decide the eligibility thresholds for CHIP, but the majority of states (48 states and the District of Columbia) set that threshold at 140 percent of the FPL or more for children. CHIP can also cover care for pregnant women but that coverage is more variable.
Differences in Coverage for Medicaid and CHIP
Federal regulations mandate Medicaid offer specific services to its covered children. This includes Early and Periodic Screening, Diagnosis and Treatment (EPSDT), comprehensive services which focus on preventive care and wellness. It includes the following:
Services also covered by Medicaid include care provided at Federally Qualified Health Centers (FQHCs) as well as rehabilitation services.
CHIP programs, however, do not have to meet the standard set by EPSDT, although they must provide benchmark care that includes hospital care, laboratory studies, X-rays, and well-child examinations, including immunizations.
Dental care may not be as extensive as that offered under EPSDT but must be part of the included benefit package. To this end, each state can choose their dental benefit based on the most popular state employee dental plan, the most popular federal employee dental plan for dependents, or coverage from the most popular commercial insurance plan in the state.
Federal Funding for Medicaid
When it comes to Medicaid, the federal government matches state spending "dollar for dollar," at least in concept. It uses what are known as Federal Medical Assistance Percentages (FMAP) to determine how much it will pay. FMAPs take into account a state's average income relative to the national average.
Each state is given an FMAP of at least 50 percent, i.e. the federal government pays 50 percent of Medicaid costs. All other states receive a higher percentage of Medicaid funds based on their calculated FMAP. With the lowest per capita income level, Mississippi will have a 2021 FMAP of 77.76% so that the federal government contributes $3.50 for every $1 the state spends.
In order to get federal Medicaid funding, the states agree to certain terms. The state is not permitted to put people on waiting lists, it cannot have an enrollment cap, and it cannot charge for premiums or copayments for anyone earning less than 150 percent of the FPL.
Federal Funding for CHIP
Federal funding for CHIP, on the other hand, has pre-set limits. Each state is given an allotment every year as a block grant. The dollar amount is fixed regardless of the number of people covered by the program.
The 50 states and the District of Columbia have a choice to use their block grants in one of three ways:
To encourage states to participate in CHIP, the federal government offers a higher matching rate than it does for Medicaid. This is referred to as the enhanced Federal Matching Assistance Percentages (eFMAP). The minimum for Medicaid matching in 2020 is 50 percent but all states are 65% or higher. Again, states with higher economic needs get reimbursed at an even higher rate.
Those states using combination programs or Medicaid expansion have the same program requirements as traditional Medicaid. States with separate CHIP programs, however, have more wiggle room. If need be, they can put children on waiting lists or establish enrollment caps to rein in CHIP costs. Many of those states will also charge premiums and copayments to their beneficiaries.
Potential Cuts to Medicaid Funding
The Trump administration attempted to repeal the Affordable Care Act and replace it with the American Health Care Act, subsequently known as the Better Care Reconciliation Act (BCRA) in 2017. This legislation did not pass but it would have ended Medicaid expansion and would have also changed how Medicaid was funded. According to the Congressional Budget Office, the BRCA would have cut $756 billion from Medicaid over a decade and 15 million people on Medicaid would have lost coverage as a result.
The BCRA did offer tax credits for individuals and families. In this way, it can be argued that attempts were made to decrease the cost of health care to Americans. Specifically, the BCRA would have replaced the ACA-income-based tax credits with a flat tax credit adjusted for age. In some cases, the subsidies would be greater under the BCRA than the ACA, but these subsidies were capped at $14,000 per year regardless of family size. Also, anyone who was eligible for an employer-sponsored health plan, Medicare, Medicaid or CHIP, or TriCare, would not have been eligible for those tax credits.
Attempts are still underway to repeal the Affordable Care Act. With the individual mandate deemed unconstitutional in 2017, a federal court judge in Texas ruled in 2018 that the Affordable Care Act as a whole is unconstitutional. That ruling is under appeal and may eventually make its way to the Supreme Court. Until then, the Affordable Care Act remains in effect.
Repealing the Affordable Care Act is not the only way to affect Medicaid coverage. The FY 2019 budget proposal, which did not pass, looked to cut Medicare by $236 billion over 10 years, affecting millions of people who are dual-eligible for Medicare and Medicaid. It would also have changed federal funding for Medicaid. By turning to block grants or per capita limits, it is estimated Medicaid would have lost $1.4 trillion by 2028.
If states were unable to make up the difference in federal funding, they would be more likely to cut benefits and limit eligibility. The neediest American families could lose their access to health care. At this time, the Trump administration has not yet put forth a new plan that would replace the Affordable Care Act if it were to be repealed. It is anticipated that a plan will be proposed in the near future.
Potential Cuts to CHIP Funding
CHIP has struggled to maintain its funding too. Federal funding for the program was set to expire in September 2017. Congress approved a stop-gap measure in December 2017 to extend funding into March 2018. It was not until January 2018 that Congress passed a more long-term solution, a retroactive six-year extension through 2023.
That very same legislation also decreases the federal matching rate over time. Any enhanced FMAP rates for CHIP that were established by the Affordable Care Act would be reduced to the regular federal match rate by 2021. With less money put into the program, fewer children may be covered.
While block grants are currently used for the CHIP program, the CHIP program is significantly smaller in scale than Medicaid. Block grants limit how many children can be covered under the CHIP program. This explains why 15 states currently have waiting lists for CHIP.
In May 2018, the White House presented a rescission proposal that would cut $7 billion from CHIP. The proposal was not approved by Congress.
A Word From Verywell
Children raised in low-income families deserve the same quality health care as their higher-earning counterparts. Medicaid offers care to the poorest families while CHIP extends coverage to a larger number of children. Care through the Medicaid program may be more extensive, but the CHIP program also offers a broad depth of coverage. Understand the difference between these two programs and make the most of your child's health care. To learn more about your state programs, visit the Medicaid site.